Behavioral health providers might consider these stressors in three categories:
1. Internal: Stressors may arise when LGBTQ+ people first notice that their gender identity doesn’t match societal or family expectations, which can result in feelings of self-loathing or self-inflicted stigma. Teens may wish they are not who they are, despite an inability to change. Substance use may begin as a mechanism to cope, quiet an internal monologue, or gain a sense of control during a time when they have little control over bodily changes.
2. External: LGBTQ+ people may feel that they cannot live their full truth. Once young adults live on their own, they gain greater freedom and control but may worry about how they are perceived by their peers and employers, fearing job loss or exclusion. Places generally considered to be safe might include bars, clubs, or social settings where alcohol and substances are readily available. For those who are genetically or socially prone to substance use issues, it can be much harder to stay sober.
3. Macro/societal: On a larger scale, minority stress means that LGBTQ+ people are marginalized based on structural and societal norms, including in ways that heterosexual populations might not ever even consider. Micro and macro aggressions are chronic and repeated. The resulting stigma and shame can persist and may be alleviated by substance use that can rapidly escalate.
Providers can help by working to understand these stressors, creating an environment that is safe and welcoming, and recognizing when their patients may need a higher level of care.
“Making changes like having gender neutral bathrooms and ensuring that resources or handouts are inclusive can make patients feel safer and more comfortable in the treatment environment,” says Nechay.
Given the chronic nature of minority stress, Nechay also notes that focusing on eradicating it may not be productive. Rather, she recommends thinking creatively about tools that can increase the ability to cope in place of substance use.
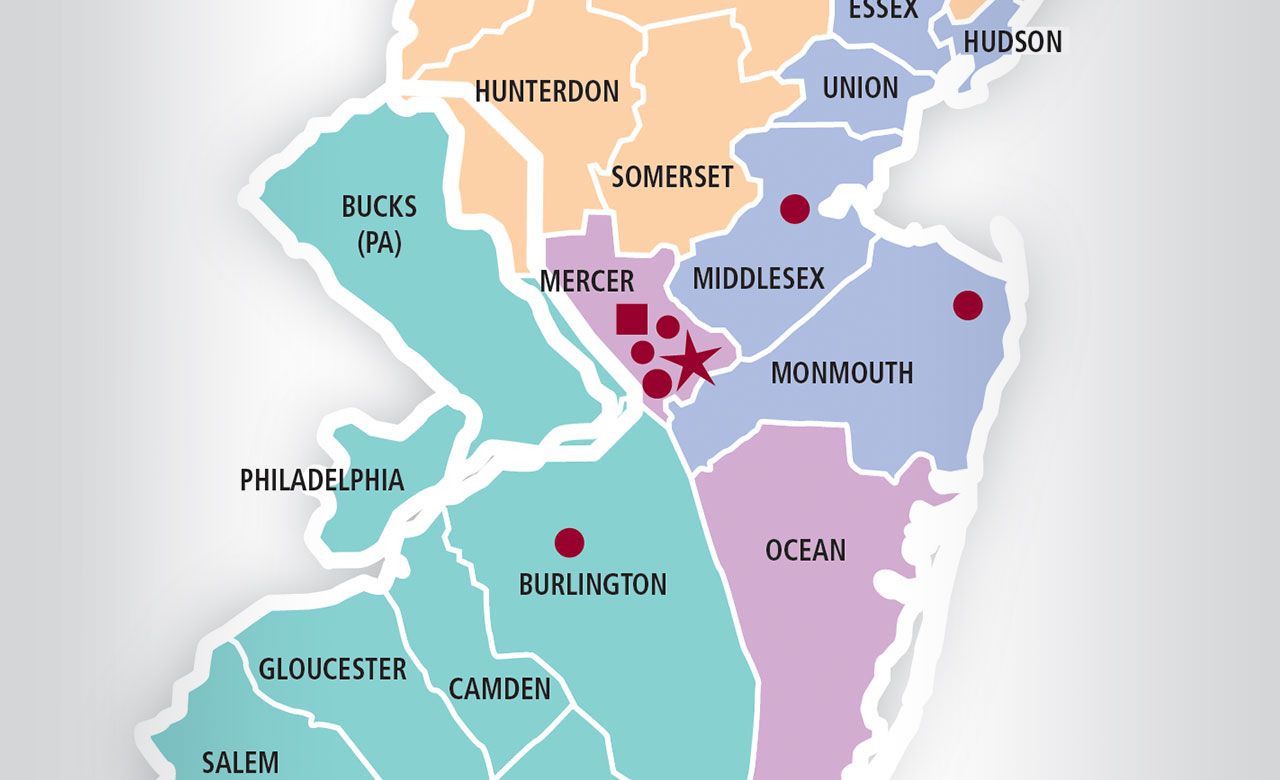
“This can be achieved on two fronts: by helping patients identify what nourishes them as individuals, and what they can safely do with others that doesn’t revolve around substances,” adds Nechay. “For populations who are already marginalized, it’s so important to find a sense of self and of community. If a higher level of care is needed, Princeton House offers trauma, dual diagnosis, and safe space programming that places honor and respect at the center of our treatment efforts.”
Article as seen in the Winter 2022 issue of Princeton House Behavioral Health Today.